ATAXIA
What is Ataxia?
Ataxia is a degenerative disease of the nervous system particularly in the cerebellum, the part of the brain that controls the coordination of movement. Damage to the cerebellum and degeneration or loss of nerves cells brings about this condition.
What causes Ataxia?
Common causes of Ataxia are the following:
- Hereditary – a defect in a certain gene that makes abnormal proteins. The abnormal proteins hamper the function of nerve cells, primarily in your cerebellum and spinal cord, and cause them to degenerate.
- Head trauma
- Stroke – severe reduction or interruption of blood flow to the brain, depriving the brain tissue of oxygen and nutrients
- Cerebral palsy
- Autoimmune diseases – examples are Multiple Sclerosis, Sarcoidosis, celiac disease and others
- Tumor – A growth on the brain, cancerous (malignant) or noncancerous (benign), can damage the cerebellum
- Alcohol and drug intoxication, heavy metal poisoning
Signs and Symptoms of Ataxia
Ataxia symptoms vary by person as well as rate of progression. Symptoms may worsen slowly, over decades or quickly, over a few months.
- Poor coordination
- Slurred speech
- Difficulty eating and swallowing
- Deterioration of fine motor skills such as feeding self or buttoning a shirt
- Unsteady gait, difficulty walking
- Abnormalities in eye movements
- Tremors
Role of Functional Medicine in Ataxia
Functional Medicine aims to support the patient in improving their quality of life through an individualized approach. And since Ataxia results from many possible causes, a thorough investigation of underlying triggers and other related conditions is done to come up with the best possible treatment plan addressing the specific needs of the patients. Apart from nutrition modification and supplementation, Ataxia responds well to intensive physical therapy, Hyperbaric Oxygen Therapy, Fecal Microbiota Transplantation for gastric problems, and DFPP.
Please click here to send us inquiry for free online consultation with our medical team.
- Published in Neurological Rehabilitation Center, Services
Traumatic Brain Injury
Traumatic Brain Injury
Traumatic brain injury usually results from a violent blow or jolt to the head or body. An object that penetrates brain tissue, such as a bullet or shattered piece of skull, also can cause traumatic brain injury.
Mild traumatic brain injury may affect your brain cells temporarily. More-serious traumatic brain injury can result in bruising, torn tissues, bleeding and other physical damage to the brain. These injuries can result in long-term complications or death.
Symptoms
Traumatic brain injury can have wide-ranging physical and psychological effects. Some signs or symptoms may appear immediately after the traumatic event, while others may appear days or weeks later.
Mild traumatic brain injury
The signs and symptoms of mild traumatic brain injury may include:
● Physical symptoms such as Loss of consciousness for a few seconds to a few minutes, No loss of consciousness, but a state of being dazed, confused or disoriented, Headache, Nausea or vomiting, Fatigue or drowsiness, Problems with speech, Difficulty sleeping, Sleeping more than usual, Dizziness or loss of balance
● Sensory symptoms such as Sensory problems, Sensitivity to light or sound, Cognitive or mental symptoms, Memory or concentration problems, Mood changes or mood swings, Feeling depressed or anxious
Moderate to severe tr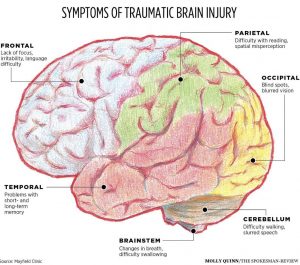 aumatic brain injuries
aumatic brain injuries
Moderate to severe traumatic brain injuries can include any of the signs and symptoms of mild injury, as well as these symptoms that may appear within the first hours to days after a head injury.
Children’s symptoms
Infants and young children with brain injuries might not be able to communicate headaches, sensory problems, confusion and similar symptoms. In a child with traumatic brain injury, you may observe change in eating or nursing habits, unusual or easy irritability, persistent crying and inability to be consoled, change in ability to pay attention, change in sleep habits, seizures, sad or depressed mood, drowsiness, loss of interest in favorite toys or activities
Causes
Traumatic brain injury is usually caused by a blow or other traumatic injury to the head or body. The degree of damage can depend on several factors, including the nature of the injury and the force of impact. Common events causing traumatic brain injury include falls, vehicle-related collisions, violence, sports injuries, explosive blasts and other combat injuries
Risk factors
The people most at risk of traumatic brain injury include:
● Children, especially newborns to 4-year-olds
● Young adults, especially those between ages 15 and 24
● Adults age 60 and older
● Males in any age group
Complications
Several complications can occur immediately or soon after a traumatic brain injury. Severe injuries increase the risk of a greater number and more-severe complications including;
● Altered consciousness
● Physical complications
● Intellectual problems
● Communication problems
● Behavioral changes
● Emotional changes
● Sensory problems
● Degenerative brain diseases
Surgical Lesions
When discussing TBI, the term “mass lesion” is often used. This refers to an area of localized injury that may cause pressure within the brain. The most common mass lesions related to TBI are hematomas and contusions. Furthermore TBI includes diffuse injuries and skull fractures.
Diagnosis
Like all trauma patients, persons with TBI need to undergo a systematic yet rapid evaluation in the emergency room. Cardiac and pulmonary function is assessed first. Next, a quick examination of the entire body is performed, followed by a complete neurological examination. The neurological examination includes an assessment utilizing the Glasgow Coma Scale (GCS). In addition to the GCS, the ability of the pupils to become smaller in bright light is also tested and also brainstem reflexes including gag and corneal (blink) may also be tested.
Radiological Tests
A computed tomography scan (CT or CAT scan) is the gold standard for the radiological assessment of a TBI patient. A CT scan is easy to perform and is an excellent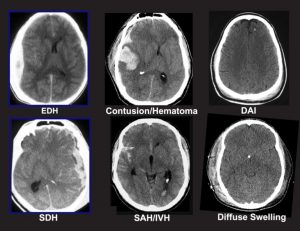 test for detecting the presence of blood and fractures, which are the most crucial lesions to identify in medical trauma cases. Plain x-rays of the skull are recommended by some as a way to evaluate patients with only mild neurological dysfunction. Magnetic resonance imaging (MRI) is not commonly used for acute head injury. However, after a patient has been stabilized, MRI may demonstrate the existence of lesions that were not detected on the CT scan. This information is generally more useful for determining prognosis than for influencing treatment.
test for detecting the presence of blood and fractures, which are the most crucial lesions to identify in medical trauma cases. Plain x-rays of the skull are recommended by some as a way to evaluate patients with only mild neurological dysfunction. Magnetic resonance imaging (MRI) is not commonly used for acute head injury. However, after a patient has been stabilized, MRI may demonstrate the existence of lesions that were not detected on the CT scan. This information is generally more useful for determining prognosis than for influencing treatment.
Surgical Treatment
Many patients with moderate or severe head injuries are taken directly from the emergency room to the operating room. In many cases, surgery is performed to remove a large hematoma or contusion that is significantly compressing the brain or raising the pressure within the skull. After surgery, these patients are usually observed and monitored in the intensive care unit (ICU).
Medical Treatment
At the present time, there is no medication or “miracle treatment” that can be given to prevent nerve damage or promote nerve healing after TBI. The primary goal in the ICU is to prevent any secondary injury to the brain. The “primary insult” refers to the initial trauma to the brain, whereas the “secondary insult” is any subsequent development that may contribute to neurological injury. For example, an injured brain is especially sensitive and vulnerable to decreases in blood pressure that might otherwise be well tolerated. One way of avoiding secondary insults is to try to maintain normal or slightly elevated blood pressure levels. Likewise, increases in ICP, decreases in blood oxygenation, increases in body temperature, increases in blood glucose and many other disturbances can potentially worsen neurological damage. The prevention of secondary insults is a major part of the ICU management of head- injured patients.
Outcome
One of the most widely used systems to classify outcome from head injury is the Glasgow Outcome Scale (GOS). Patients with mild head injury (usually defined as GCS score on admission of 13-15) tend to do well. They may experience headaches, dizziness, irritability or similar symptoms, but these gradually improve in most cases.
Patients with moderate head injuries fare less well. Approximately 60 percent will make a positive recovery, and an estimated 25 percent will be left with a moderate degree of disability. Death or a persistent vegetative state will be the outcome in about 7 to 10 percent of cases. The remainder of patients will have a severe degree of disability.
Rehabilitation
Once head-injured patients leave the acute-care hospital, some may benefit from a rehabilitation program. Prime candidates for rehabilitation are patients that had less severe initial injuries or those that have started to show significant improvement. In some cases, further recovery may be expedited by transfer to a rehabilitation hospital or to the rehabilitation service of a large hospital. For more severely injured patients or for those whose recovery is slow, constant vigilance is required to prevent the gradual onset of problems with joint mobility, skin integrity, respiratory status, infection and many other physiological functions. Patients with moderate or mild injuries, as well as severely injured patients who have improved sufficiently, may be candidates for outpatient therapy.
Prevention
To reduce the risk of brain injury you should wear a belt when driving. A small child should always sit in a child seat and install it in the back seat. Also, you should wear a helmet when riding a motorcycle, bicycle or playing sports such as skateboarding, snowmobile, or all-terrain vehicle. To protect the head in the event of an accident.
● Preventing falls can help older adults avoid falls around the house such as Install handrails in bathrooms, Put a nonslip mat in the bathtub or shower, Install handrails on both sides of staircases, Improve lighting in the home, Keep stairs and floors clear of clutter.
● Preventing head injuries in children such as Install safety gates at the top of a stairway, Keep stairs clear of clutter, Install window guards to prevent falls, Put a nonslip mat in the bathtub or shower, Use playgrounds that have shock-absorbing materials on the ground, Make sure area rugs are secure, Don’t let children play on fire escapes or balconies.
- Published in Neurological Rehabilitation Center, Services
STROKE
What is Stroke?
Stroke is a medical emergency that occurs when blood supply to the brain is interrupted or cut off due to a blockage (ischemic stroke) or a rupture of the blood vessel (hemorrhagic stroke). Bleeding and deprivation of the brain from oxygen results in brain tissue damage and brain cell death. Stroke however, can be treated and prevented.
Current diagnostic methods are highly effective and are able to identify the location of the damage or abnormalities in the brain or blood vessels, as well as any conditions and causes that could be risk factors for an impending stroke.
What are the signs and symptoms of Stroke?
- Sudden numbness or weakness on one side of the body
- Sudden confusion
- Sudden difficulty in speaking or understanding speech
- Sudden vision impairment on one or both eyes
- Sudden trouble walking, dizziness or loss of balance
- Sudden severe headache with unknown cause
What is the role of Functional Medicine in Stroke?
Stroke is highly treatable and post-stroke patients have a high chance of recovering from complications and disabilities. Functional Medicine comes in to help improve one’s symptoms through a thorough investigation, holistic rehabilitation, biochemistry work up, nutritional enhancement, supportive therapies, and other possible treatments that aid in healing the actual brain injury. Stroke may also have a tendency to recur. Because of this, Functional Medicine enables patients with the necessary preventive knowledge and measures to boost their overall health considering their identified risk factors.
- Published in Neurological Rehabilitation Center, Services
Spina Bifida
- Published in Neurological Rehabilitation Center, Services
Parkinson disease
Parkinson’s disease is a progressive nervous system disorder that affects movement. Symptoms start gradually, sometimes starting with a barely noticeable tremor in just
one hand. Tremors are common, but the disorder also commonly causes stiffness or slowing of movement.
Sign and symptom
Parkinson’s signs and symptoms may include:
- Tremor, or shaking, usually begins in a limb, often your hand or fingers. You may rub your thumb and forefinger back-and-forth, known as a pill-rolling tremor.
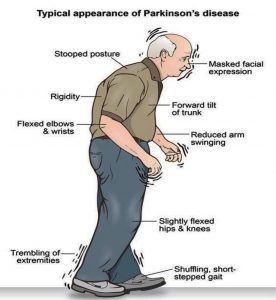 Your hand may tremor when it’s at rest.
Your hand may tremor when it’s at rest. - Slowed movement (bradykinesia), Over time, Parkinson’s disease may slow your movement, making simple tasks difficult and time-consuming. Your steps may become shorter when you walk. It may be difficult to get out of a chair. You may drag your feet as you try to walk.
- Rigid muscles, Muscle stiffness may occur in any part of your body. The stiff muscles can be painful and limit your range of motion.
- Impaired posture and balance, Your posture may become stooped, or you may have balance problems as a result of Parkinson’s disease.
- Loss of automatic movements, You may have a decreased ability to perform unconscious movements, including blinking, smiling or swinging your arms when you walk.
- Speech changes, You may speak softly, quickly, slur or hesitate before talking. Your speech may be more of a monotone rather than with the usual inflections.
- Writing changes, It may become hard to write, and your writing may appear small.
Causes
In Parkinson’s disease, certain nerve cells (neurons) in the brain gradually break down or die. Many of the symptoms are due to a loss of neurons that produce a chemical messenger in your brain called dopamine. When dopamine levels decrease, it causes abnormal brain activity, leading to symptoms of Parkinson’s disease. The cause of Parkinson’s disease is unknown, but several factors appear to play a role, including:
- Your genes.
- Environmental triggers.
- The presence of Lewy bodies.
- Alpha-synuclein is found within Lewy bodies.
Risk factors
Risk factors for Parkinson’s disease include:
- Age, Young adults rarely experience Parkinson’s disease. It ordinarily begins in middle or late life, and the risk increases with age. People usually develop the disease around age 60 or older.
- Heredity, Having a close relative with Parkinson’s disease increases the chances that you’ll develop the disease. However, your risks are still small unless you have many relatives in your family with Parkinson’s disease.
- Sex, Men are more likely to develop Parkinson’s disease than are women.
- Exposure to toxins. Ongoing exposure to herbicides and pesticides may slightly increase your risk of Parkinson’s disease.
Complications
Parkinson’s disease is often accompanied by these additional problems, which may be treatable: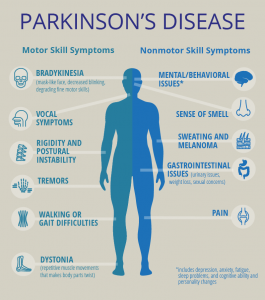
- Thinking difficulties.
- Depression and emotional changes.
- Swallowing problems.
- Chewing and eating problems.
- Sleep problems and sleep disorders.
- Bladder problems.
- Constipation.
You may also experience:
- Blood pressure changes.
- Smell dysfunction.
- Pain.
- Sexual dysfunction.
Diagnosis
A physician will initially assess for Parkinson’s disease with a careful medical history and neurological examination. People may be given levodopa, with any resulting improvement in motor impairment helping to confirm the PD diagnosis. Other causes that can secondarily produce parkinsonism are stroke and drugs.
Medical organizations have created diagnostic criteria to ease and standardize the diagnostic process, especially in the early stages of the disease. The Queen Square Brain Bank criteria require slowness of movement (bradykinesia) plus either rigidity, resting tremor, or postural instability. Other possible causes of these symptoms need to be ruled out. Finally, three or more of the following supportive features are required during onset or evolution: unilateral onset, tremor at rest, progression in time, asymmetry of motor symptoms, response to levodopa for at least five years, clinical course of at least ten years and appearance of dyskinesias induced by the intake of excessive levodopa.
Imaging
Computed tomography (CT) scans of people with PD usually appear normal. MRI has become more accurate in diagnosis of the disease which can demonstrate absence of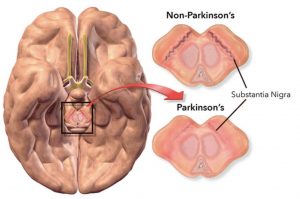 the characteristic ‘swallow tail’ imaging pattern in the dorsolateral substantia nigra. In a meta-analysis, absence of this pattern was highly sensitive and specific for the disease. Diffusion MRI has shown potential in distinguishing between PD and Parkinson plus syndromes, though its diagnostic value is still under investigation. CT and MRI are also used to rule out other diseases that can be secondary causes of parkinsonism.
the characteristic ‘swallow tail’ imaging pattern in the dorsolateral substantia nigra. In a meta-analysis, absence of this pattern was highly sensitive and specific for the disease. Diffusion MRI has shown potential in distinguishing between PD and Parkinson plus syndromes, though its diagnostic value is still under investigation. CT and MRI are also used to rule out other diseases that can be secondary causes of parkinsonism.
The metabolic activity of dopamine transporters in the basal ganglia can be directly measured with PET and SPECT scans, with the DaTSCAN. It has shown high agreement with clinical diagnoses of Parkinson’s. Reduced dopamine-related activity in the basal ganglia can help exclude drug-induced Parkinsonism. This finding is not entirely specific, however, and can be seen with both PD and Parkinson-plus disorders.
Treatment
Parkinson’s disease can’t be cured, but medications can help control your symptoms, often dramatically. In some later cases, surgery may be advised. Your doctor may also recommend lifestyle changes, especially ongoing aerobic exercise. In some cases, physical therapy that focuses on balance and stretching also is important. A speech-language pathologist may help improve your speech problems.
- Medications
Medications may help you manage problems with walking, movement and tremor. These medications increase or substitute for dopamine. People with Parkinson’s disease have low brain dopamine concentrations. However, dopamine can’t be given directly, as it can’t enter your brain. You may have significant improvement of your symptoms after beginning Parkinson’s disease treatment. Over time, however, the benefits of drugs frequently diminish or become less consistent. You can usually still control your symptoms fairly well.
- Surgical procedures
Deep brain stimulation. In deep brain stimulation (DBS), surgeons implant electrodes into a specific part of your brain. The electrodes are connected to a generator implanted in your chest near your collarbone that sends electrical pulses to your brain and may reduce your Parkinson’s disease symptoms.
- Lifestyle and home remedies
If you’ve received a diagnosis of Parkinson’s disease, you’ll need to work closely with your doctor to find a treatment plan that offers you the greatest relief from symptoms with the fewest side effects. Certain lifestyle changes also may help make living with Parkinson’s disease easier.
- Healthy eating
While no food or combination of foods has been proved to help in Parkinson’s disease, some foods may help ease some of the symptoms. For example, eating foods high in fiber and drinking an adequate amount of fluids can help prevent constipation that is common in Parkinson’s disease. A balanced diet also provides nutrients, such as omega-3 fatty acids, that might be beneficial for people with Parkinson’s disease.
- Exercise
Exercising may increase your muscle strength, flexibility and balance. Exercise can also improve your well-being and reduce depression or anxiety such as walking, swimming, gardening, dancing, water aerobics or stretching etc.
- Published in Neurological Rehabilitation Center, Services
Multiple Sclerosis
MULTIPLE SCLEROSIS (MS)
What is MS?
MS is an unpredictable autoimmune condition affecting the brain and spinal cord. The body attacks the protective sheath (myelin) that covers the nerve fibers. When the myelin sheath is damaged or destroyed, this can severely slow the process of transmitting information from the brain to the body. It can range from being benign
What are the signs and symptoms?
- Numbness or weakness in one or more limbs that typically occurs on one side of your body at a time, or the legs and trunk
- Electric-shock sensations that occur with certain neck movements
- Tremor, lack of coordination or unsteady gait
- Vision – partial or complete loss of vision (usually in one eye at a time), prolonged double vision, blurry vision
- Slurred speech
- Fatigue
- Dizziness
- Problems with sexual, bowel and bladder function
How is MS diagnosed?
There are no specific tests to diagnose MS but the doctor may rule out other conditions that have similar signs and symptoms. A series of tests and screening exams, medical history and thorough assessment helps in the diagnosis.
Role of Functional Medicine in MS
Functional Medicine is directed towards the underlying causes of the patient’s symptoms by addressing inflammation issues. The main goal is to enhance the body’s ability to care for itself and to support the immune system as a whole, reduce symptoms or delay the development of the disease.
The treatment plans vary per patient and their specific symptoms. Common approach would include nutritional assessment and revision of the patient’s diet, detect digestive problems and treat with FMT, eliminating possible toxins in the blood through antioxidants treatment, identifying infections, and appropriate physiotherapy activities.
- Published in Neurological Rehabilitation Center, Services
CEREBRAL PALSY (CP)
CEREBRAL PALSY (CP)
What is CP?
Cerebral Palsy is a combination of problems that affects ones muscle tone, movement and motor skills. A person with CP does not have coordination of movement. It can affect other basic but essential body functions such as breathing, bladder and bowel control, eating and talking. It often stems from brain damage that occurs before or during birth or from 3-5 years of a child’s life. Conditions like vision, hearing and learning problems may arise from CP. However, it does not progress or get worse over time.
What causes CP?
There is no definite cause. It happens during the brain’s development. It may be due to one factor or a combination of many issues. Some known factors that contribute to CP are:
- infections during pregnancy
- brain damage due to several causes such as injuries or meningitis
- complications in premature birth (poor blood flow to the brain)
- untreated jaundice
- mother’s medical problems during pregnancy
What are the types of CP?
- Spastic Cerebral Palsy — most common. Decreased muscle tone causes stiffness and jerky movements.
- Dyskinetic – characterized by uncontrolled movements that can be twisting, repetitive, slow, or unpredictable. Can be very severe.
- Ataxic – characterized by shaky movements that affects balance, coordination, posture positioning and even eye movements.
Role of Functional Medicine in CP
The goal in CP patients is to assist in improving brain and neurological function and improve symptoms. Integrative and customized neuro-regenerative programs are designed for each patient depending on their condition. Adjuvant therapies can also be identified and combined with our physiotherapy programs such as Robotics Training, G-Factor and Transcranial Magnetic Stimulation.
- Published in Neurological Rehabilitation Center, Services
Spinal bifida
Introduction: Spina bifida is a condition that affects the spine and is usually apparent at birth. It is a type of neural tube defect (NTD).
Spina bifida can happen anywhere along the spine if the neural tube does not close all the way. When the neural tube doesn’t close all the way, the backbone that protects the spinal cord doesn’t form and close as it should. This often results in damage to the spinal cord and nerves.
Spina bifida might cause physical and intellectual disabilities that range from mild to severe. The severity depends on:
- The size and location of the opening in the spine.
Whether part of the spinal cord and nerves are affected.
Causes of spina bifida
The cause of spina bifida is unknown, but a number of factors can increase the risk of a baby developing the condition.
These include:
- low folic acid intake during pregnancy
- having a family history of spina bifida
- medication – taking certain medications during pregnancy has been linked to an increased risk of having a baby with spina bifida
Sign and Symptom: Types of Spina Bifida
The three most common types of spina bifida are Myelomeningocele (sounds like: my-low-ma-nin-jo-seal; hear how “myelomeningocele” sounds
When people talk about spina bifida, most often they are referring to myelomeningocele. Myelomeningocele is the most serious type of spina bifida. With this condition, a sac of fluid comes through an opening in the baby’s back. Part of the spinal cord and nerves are in this sac and are damaged. This type of spina bifida causes moderate to severe disabilities, such as problems affecting how the person goes to the bathroom, loss of feeling in the person’s legs or feet, and not being able to move the legs.
Meningocele (sounds like: ma-nin-jo-seal; hear how “meningocele” sounds
Another type of spina bifida is meningocele. With meningocele a sac of fluid comes through an opening in the baby’s back. But, the spinal cord is not in this sac. There is usually little or no nerve damage. This type of spina bifida can cause minor disabilities.
Spina Bifida Occulta (sounds like: o-cult-tuh; hear how “occulta” sounds
Spina bifida occulta is the mildest type of spina bifida. It is sometimes called “hidden” spina bifida. With it, there is a small gap in the spine, but no opening or sac on the back. The spinal cord and the nerves usually are normal. Many times, spina bifida occulta is not discovered until late childhood or adulthood. This type of spina bifida usually does not cause any disabilities.
Diagnosis: Diagnosing spina bifida
Most cases of spina bifida are detected during the mid-pregnancy anomaly scan, which is offered to all pregnant women between 18 and 21 weeks of pregnancy.
If tests confirm that your baby has spina bifida, the implications will be discussed with you.
This will include a discussion about the possible problems associated with the condition, the treatment and support your child may need if you decide to continue with the pregnancy, and what your options are regarding ending the pregnancy, if that’s your choice.
Tests after birth
Once the baby is born, a number of tests may be carried out to assess the severity of the condition and help decide which treatments are appropriate.
Tests may include:
- monitoring your child’s head growth and carrying out a brain scan, using an ultrasound scan, CT scan or MRI scan, to check for hydrocephalus (excess fluid on the brain)
- ultrasound scans of the bladder and kidneys to check whether your baby stores urine normally
- an assessment of your baby’s movements to check for paralysis
In most cases, surgery to repair the spine will be recommended soon after your baby is born.
Treating spina bifida
Treatments for the symptoms or conditions associated with spina bifida include:
- surgery soon after birth to close the opening in the spine and treat hydrocephalus
- therapies to help make day-to-day life easier and improve independence, such as physiotherapy and occupational therapy
- assistive devices and mobility equipment, such as a wheelchair, or walking aids
- treatments for bowel and urinary problems
With the right treatment and support, many children with spina bifida survive well into adulthood.
It can be a challenging condition to live with, but many adults with spina bifida are able to lead independent and fulfilling lives.
Read more about treating spina bifida
Treatment: Treatments for the symptoms or conditions associated with spina bifida include:
- surgery soon after birth to close the opening in the spine and treat hydrocephalus
- therapies to help make day-to-day life easier and improve independence, such as physiotherapy and occupational therapy
assistive devices and mobility equipment, such as a wheelchair, or walking aids
- treatments for bowel and urinary problems
With the right treatment and support, many children with spina bifida survive well into adulthood.
It can be a challenging condition to live with, but many adults with spina bifida are able to lead independent and fulfilling lives.
What Makes our Treatment for Spina Bifida Effective?
Since 2005, we have been developing comprehensive stem cell therapy protocols for Spina Bifida to overcome the limitations of conventional therapies. In our protocols, stem cells are combined with specialized therapies for spina bifida that not only focus on helping the patient to cope with their symptoms, but also treat the root cause of the condition by promoting the healing of the original spinal cord/brain injury. We believe that our comprehensive therapy approach for spina bifida gives our patients the best chances of improvements, allowing for a better quality of life.
What potential improvements after the treatment?
The purpose of the treatment is to promote healing of the original spinal cord/brain injury in order to restore neurological function. Thus, various kinds of improvement are possible after our treatment and our past patients have experienced the following*:
- Improved motor function
- Increased sensations
- Improved development
- Improved mental abilities
- Increased muscle strength
- Reduced epilepsy seizures
- Enhanced bladder & bowel function
- Published in Neurological Rehabilitation Center, Services
Muscular Dystrophy
Introduction: Muscular dystrophy is a group of diseases that cause progressive weakness and loss of muscle mass. In muscular dystrophy, abnormal genes (mutations) interfere with the production of proteins needed to form healthy muscle.
There are many different kinds of muscular dystrophy. Symptoms of the most common variety begin in childhood, mostly in boys. Other types don’t surface until adulthood.
There’s no cure for muscular dystrophy. But medications and therapy can help manage symptoms and slow the course of the disease.
Causes
Muscular dystrophy is caused by mutations on the X chromosome. Each version of muscular dystrophy is due to a different set of mutations, but all prevent the body from producing dystrophin. Dystrophin is a protein essential for building and repairing muscles.
Duchenne muscular dystrophy is caused by specific mutations in the gene that encodes the cytoskeletal protein dystrophin. Dystrophin makes up just 0.002 percent of the total proteins in striated muscle, but it is an essential molecule for the general functioning of muscles.
Dystrophin is part of an incredibly complex group of proteins that allow muscles to work correctly. The protein helps anchor various components within muscle cells together and links them all to the sarcolemma – the outer membrane.
If dystrophin is absent or deformed, this process does not work correctly, and disruptions occur in the outer membrane. This weakens the muscles and can also actively damage the muscle cells themselves.
In Duchenne muscular dystrophy, dystrophin is almost totally absent; the less dystrophin that is produced, the worse the symptoms and etiology of the disease. In Becker muscular dystrophy, there is a reduction in the amount or size of the dystrophin protein.
The gene coding for dystrophin is the largest known gene in humans. More than 1,000 mutations in this gene have been identified in Duchenne and Becker muscular dystrophy
Sign and Symptom: The main sign of muscular dystrophy is progressive muscle weakness. Specific signs and symptoms begin at different ages and in different muscle groups, depending on the type of muscular dystrophy.
Duchenne type muscular dystrophy
This is the most common form of muscular dystrophy. Although girls can be carriers and mildly affected, it’s much more common in boys.
About one-third of boys with Duchenne muscular dystrophy (DMD) don’t have a family history of the disease, possibly because the gene involved may be subject to sudden abnormal change (spontaneous mutation).
Signs and symptoms typically appear in early childhood and may include:
- Frequent falls
- Difficulty rising from a lying or sitting up position
- Trouble running and jumping
- Waddling gait
- Large calf muscles
- Walking on the toes
- Muscle pain and stiffness
- Learning disabilities
Becker muscular dystrophy
Signs and symptoms are similar to those of Duchenne muscular dystrophy, but tend to be milder and progress more slowly. Symptoms generally begin in the teens but may not occur until the mid-20s or even later.
Other types of muscular dystrophy
Some types of muscular dystrophy are defined by a specific feature or by where in the body symptoms first begin. Examples include:
Facioscapulohumeral (FSHD). Muscle weakness typically begins in the face and shoulders. The shoulder blades might stick out like wings when a person with FSHD raises his or her arms. Onset usually occurs in the teenage years but may begin in childhood or as late as age 40
- Also known as Steinert’s disease, this form is characterized by an inability to relax muscles at will following contractions. Myotonic muscular dystrophy is the most common form of adult-onset muscular dystrophy. Facial and neck muscles are usually the first to be affected.
- Limb-girdle. Hip and shoulder muscles are usually the first affected. People with this type of muscular dystrophy may have difficulty lifting the front part of the foot and as a result may trip frequently. Onset usually begins in childhood or the teenage years..
- This type affects boys and girls and is apparent at birth or before age 2. Some forms progress slowly and cause only mild disability, while others progress rapidly and cause severe impairment.
Complications
The complications of progressive muscle weakness include:
- Trouble walking. Some people with muscular dystrophy eventually need to use a wheelchair.
- Shortening of muscles or tendons around joints (contractures). Contractures can further limit mobility.
- Breathing problems. Progressive weakness can affect the muscles associated with breathing. People with muscular dystrophy may eventually need to use a breathing assistance device (ventilator), initially at night but possibly also during the day.
- Curved spine (scoliosis). Weakened muscles may be unable to hold the spine straight.
- Heart problems. Muscular dystrophy can reduce the efficiency of the heart muscle.
- Swallowing problems. If the muscles involved with swallowing are affected, nutritional problems and aspiration pneumonia may develop. Feeding tubes may be an option.
Diagnosis: There are a variety of techniques used to definitively diagnose muscular dystrophy:
The genetic mutations involved in muscular dystrophy are well known and can be used to make a diagnosis.
- Enzyme assay: Damaged muscles produce creatine kinase (CK). Elevated levels of CK in the absence of other types of muscle damage could suggest muscular dystrophy.
- Genetic testing: As genetic mutations are known to occur in muscular dystrophy, these changes can be screened for.
- Heart monitoring: Electrocardiography and echocardiograms can detect changes in the musculature of the heart. This is especially useful for the diagnosis of myotonic muscular dystrophy.
- Lung monitoring: Checking lung function can give additional evidence.
- An electrode needle is inserted into the muscle to be tested. Electrical activity is measured as you relax and as you gently tighten the muscle. Changes in the pattern of electrical activity can confirm a muscle disease.
- Genetic testing. Blood samples can be examined for mutations in some of the genes that cause different types of muscular dystrophy.
- Muscle biopsy. A small piece of muscle can be removed through an incision or with a hollow needle. Analysis (biopsy) of the tissue sample can distinguish muscular dystrophies from other muscle diseases.
Treatment:
Drugs
The two most commonly prescribed drugs for muscular dystrophy are:
- Corticosteroids: This type of medication can help increase muscle strength and slow progression, but long-term use can weaken bones and increase weight gain.
Heart medications: If the condition impacts the heart, beta blockers and angiotensin-converting enzyme (ACE) inhibitors may help
Therapy
Several types of therapy and assistive devices can improve the quality and sometimes the length of life in people who have muscular dystrophy. Examples include:
- Range-of-motion and stretching exercises. Muscular dystrophy can restrict the flexibility and mobility of joints. Limbs often draw inward and become fixed in that position. Range-of-motion exercises can help to keep joints as flexible as possible.
- Low-impact aerobic exercise, such as walking and swimming, can help maintain strength, mobility and general health. Some types of strengthening exercises also might be helpful. But it’s important to talk to your doctor first because some types of exercise might be harmful.
- Braces can help keep muscles and tendons stretched and flexible, slowing the progression of contractures. Braces can also aid mobility and function by providing support for weakened muscles.
- Mobility aids. Canes, walkers and wheelchairs can help maintain mobility and independence.
- Breathing assistance. As respiratory muscles weaken, a sleep apnea device may help improve oxygen delivery during the night. Some people with severe muscular dystrophy may need to use a machine that forces air in and out of their lungs (ventilator).
What Makes our Stem Cell Treatment for Muscular Dystrophy Effective?
Since 2005, we have been developing comprehensive protocols regarding stem cell treatment for muscular dystrophy to overcome the limitations of conventional therapies. In our protocols, stem cells are combined with specialized therapies for muscular dystrophy that not only focus on helping the patient to cope with their symptoms, but also treat the direct cause of the symptoms by promoting the healing of the affected muscles. We believe that our comprehensive stem cell treatment for muscular dystrophy gives our patients the best chances of improvements, allowing for a better quality of life. Different types of muscular dystrophy can be considered for treatment, such as Duchenne, Becker, Limb Girdle, Fascio-Scapulo Humeral and more.
What potential improvements after therapy?
The purpose of stem cell treatment for muscular dystrophy is to promote the healing and growth of the affected muscles. Thus, various kinds of improvement are possible after our treatment and our past patients have experienced the following*:
- Enlarged muscle mass
- Improved range of movement
- Increased muscle strength
- Decreased tremor occurrence
- Improved balance
- Decreased stiffness
- Improved development (in children)
- Published in Neurological Rehabilitation Center, Services
Motor Neuron Diseases
MOTOR NEURON DISEASES (MNDs)
What is Motor Neuron Disease?
MNDs are a group of rare neurological disorders that progressively damage parts of the nervous system particularly the motor neurons. Motor Neurons are cells that control vital muscle activity responsible for gripping, speaking, walking, breathing and swallowing. This leads to general muscle weakness and is visible with wasting. A disruption in the signals between motor neurons and the muscles causes the dysfunction or loss of voluntary movement.
MNDs may affect children or adults. The causes of MNDs are not clearly known. It may be inherited, or effects of environmental, toxic, viral or a collection of many factors.
Signs and Symptoms:
There are numerous signs and symptoms and usually depend on the type of MND. Early signs and symptoms include:
- weakness in ankles or legs such as easily tripping or sudden difficulty to climb stairs
- slurred speech which gradually develop into difficulty swallowing some food
- weak hand grip manifested in dropping things or difficulty opening jars or buttoning clothes
- Weakness in shoulders that cause difficulty in lifting objects
- Unexplained muscle cramps and twitches
- weight loss or thinning of muscles on arms and legs
- breathing difficulty and shortness of breath not related to common respiratory disorders
Types of Motor Neuron Diseases
- ALS or Lou Gehrig’s disease – the most common type, affecting neurons in the brain and spinal cord. Effects are manifested on the muscles of the arms, legs, mouth, and respiratory system. A person with ALS may live another 3–5 years on avergae, but with proper supportive care, some have more than 10 years.
- Primary lateral sclerosis – rare form of MND that affects the neurons in the brain and progresses slower than ALS. It can still affect a person’s quality of life but is not fatal.
- Progressive bulbar palsy (PBP) – involves the brain stem. The condition causes frequent choking spells, difficulty speaking, eating, and swallowing.
- Progressive muscular atrophy (PMA) – a rare condition that affects the lower motor neurons in the spinal cord and causes slow but progressive muscle wasting, especially in the arms, legs, and mouth.
- Spinal muscular atrophy (SMA) – is an inherited MND that afflicts children caused by a genetic change known as SMA1. It usually affects the trunk, legs, and arms.
Role of Functional Medicine in MND
Functional Medicine for MND is multi-level assessment which usually starts with testing metabolic status, evaluating imbalances at the cellular level, genetic testing, identifying risk factors of the patient’s susceptibility to this disease and to help find out why the disease has occurred in the first place. By understanding each of the imbalances identified the specialist is able to formulate and educate the patient about the most appropriate and beneficial diet and lifestyle modification. Another purpose is to promote the healing of the brain injury which can manifest in improved motor functions, balance, better coordination, decreased fatigue, increase in muscle tone and strength, and other improvements of symptoms through intensive physiotherapy, Robotics training, possible stem cell treatment and FMT.
- Published in Neurological Rehabilitation Center, Services
- 1
- 2

 ไทย
ไทย  繁體中文
繁體中文  العربية
العربية  Português
Português  Español
Español 









